Nuchal Cords: The Perfect Scapegoat



 To get this blog going I decided to write about a slight obsession of mine: The fear of, and routine midwifery management of nuchal cords at birth (umbilical cord around the neck). It was this issue that started me down the track of my PhD (which has grown and evolved since). I have written and presented about this topic and have bored the pants off many a person who has made the mistake of mentioning the subject. So, despite telling my colleagues that I had put away my ‘nuchal cord’ soap box I am bringing it out to launch this blog. The content of this post is based on a literature review I carried out. If you are interested in finding out more, or seeing the reference sources for the following information you can download a journal article here or the full literature review here.
To get this blog going I decided to write about a slight obsession of mine: The fear of, and routine midwifery management of nuchal cords at birth (umbilical cord around the neck). It was this issue that started me down the track of my PhD (which has grown and evolved since). I have written and presented about this topic and have bored the pants off many a person who has made the mistake of mentioning the subject. So, despite telling my colleagues that I had put away my ‘nuchal cord’ soap box I am bringing it out to launch this blog. The content of this post is based on a literature review I carried out. If you are interested in finding out more, or seeing the reference sources for the following information you can download a journal article here or the full literature review here.
Why and how babies end up wearing their cord around their neck
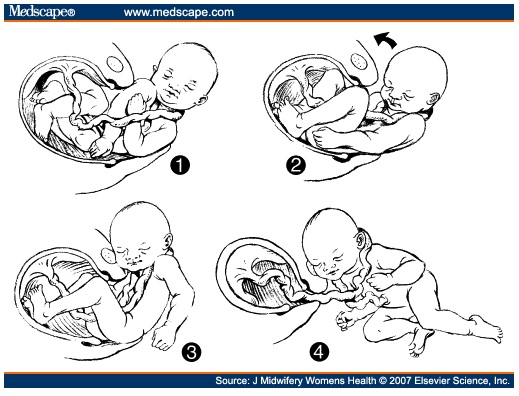
The presence of a nuchal cord is a very common occurrence during birth. Around a third of all babies are born with the umbilical cord around their neck. How and when it ends up there will be different for individual babies. Interestingly it is more common with boy babies – perhaps because they are more likely to have longer cords. It also becomes more common with increasing gestation – I suppose there is more time to get wrapped the cord. If a nuchal cord does not occur in pregnancy it can occur during labour. As the baby moves through the pelvis he/she rotates and can spin the cord around their neck. See this post to see how rotation works.
A versatile scapegoat
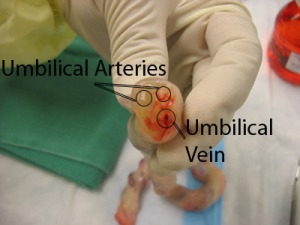 Image credit: http://homepages.cae.wisc.edu/~bme300/umbilical_f07/
Image credit: http://homepages.cae.wisc.edu/~bme300/umbilical_f07/
The nuchal cord has become the perfect scapegoat because it lays blame with the mother/baby rather than the careprovider/system. The result is that fear about nuchal cords is embedded within our culture. Whenever I read a story about an unexpected birth outside of hospital it always seems to involve a nuchal cord. The story being about how lucky the baby was to survive the dangers of a nuchal cord away from the experts who can manage such a complication. In addition, I have heard too many birth stories where the resulting complications were blamed on the presence of a nuchal cord.
Before I tackle some of the myths – some quick anatomy and physiology: The umbilical cord is designed to be worn around the neck without causing a problem. The cord is covered in Wharton’s jelly and coiled. This protects the 3 blood vessels from the kind of stretch and compression involved in being attached to a mobile baby. The umbilical cord is also long enough (average 55cm) to be comfortably wrapped around the neck with plenty of left over length.
Pregnancy
There is no research to support the idea that nuchal cords are associated with babies dying during pregnancy. Unfortunately some babies do not make it, and die before labour begins. There is often no known reason for this which can add to the devastation. When these babies are born they are often found to have the cord around their neck (like a 3rd of all babies). Although I can understand the need to find a reason and to pick the obvious, I don’t think this is helpful in the longer term. Parents need honest answers about the loss of their baby, even if the answer is ‘we don’t know’.
Labour
During labour a nuchal cord does not cause a problem. The baby is not ‘held up’ by the cord because the whole package – fundus (top of the uterus), placenta and cord are all moving down together. The uterus ‘shrinks’ down (contracts) moving the baby downwards, along with their attached placenta and cord. It is not until the baby’s head moves into the vagina that a few extra centimetres of additional length are required (see ‘birth’ below). However, when a c-section is done for ‘fetal distress’ or ‘lack of progress’ during labour, the presence of a nuchal cord is often used as the reason… “ah ha, look – your baby was stressed because the cord was around his neck” or “…the cord was stopping her from moving down”. The cord is unlikely to have had anything to do with the stress or lack of progress. Most likely other interventions carried out during labour led to the end scenario (eg. the use of syntocinon and/or ‘failure to wait’).
Birth (the last bit of labour)
The nuchal cord remains around the baby’s neck as his head moves out of the uterus and through the vagina. Usually the cord remains loose as there is lots of ‘give’ in it. A loose nuchal cord does not cause any problems. Blood continues to flow through the vessels just as it did during pregnancy and labour.
Occasionally a cord becomes stretched and tight during this last bit of labour – as the head is born. Either there is not enough ‘give’, or the cord is trapped against the pelvis by the baby’s body. This may happen with a shorter than average cord that is wrapped around the neck a number of times. However, the baby is not ‘strangled’ because he/she is not breathing oxygen. Their oxygen is provided by the cord, not their airway. Whilst the cord is stretched and compressed the blood vessels transfer less blood (but still some). This results in short-term hypoxia (reduced oxygen supply) which resolves once the cord is loosened after birth and full blood flow resumes. These babies may arrive a little compromised but quickly recover – if the cord is left alone. Unfortunately the way in which the situation is managed (see below) can create further problems. The resulting need for resuscitation is then blamed on the nuchal cord rather than what was done to it by the care provider.
Risks associated with clamping and cutting a tight nuchal cord
Once the cord is clamped, blood flow between the baby and placenta ceases, reducing the baby’s blood volume and oxygen supply. This makes resuscitation more necessary and difficult once the baby is born. Any delay in the birth of the baby (eg. shoulder dystocia will further increase the risk of hypoxia. While waiting to be born the baby now has NO blood supply rather than a limited one. There have been successful malpractice actions against obstetricians in the US who cut nuchal cords prior to shoulder dystocia.
One study (Sadan et al. 2007) found that neither cutting nor leaving a nuchal cord adversely affected the outcome for babies. However, they did not look at tight nuchal cords, and the cords were cut after the anterior shoulder had birthed.
For a baby with a tight nuchal cord the worst thing you can do is clamp and cut!
Risks associated with pulling and looping a loose nuchal cord
A far more common practice is pulling and looping a loose nuchal cord. Most care providers do this and I was taught to do this when I trained. However, handling the cord stimulates the umbilical arteries to vasoconstrict reducing blood flow. Loosening the cord will usually involve some traction which can risk tearing the cord and subsequent bleeding (from the baby). As a student midwife I snapped a cord while looping it over the baby’s head. Luckily my mentor clamped the ends quickly but not before I got blood sprayed in my eyes! I later discovered that babies can be born with the cord around their neck. They either birth through the loop or they come out with it still wrapped.
Checking for a nuchal cord
So, if you are not going to cut or loop a nuchal cord what’s the point in digging about to see if it is there? Checking for a cord interferes with the physiological process of birth. It also reinforces the notion that this is a birth complication that endangers the baby, rather than a common situation. Telling the woman to stop pushing and putting your fingers into her vagina can be disempowering and painful.
Suggestions
▪ Talk to parents before birth about the possibility and normalcy of a nuchal cord.
▪ During birth DO NOTHING.
▪ IF the cord is preventing the baby descending once the head is born (extremely rare) use the ‘somersault technique’ (Schorn & Blanco 1991) – see below.
▪ Once the baby is born unwrap the cord (the mother/family can do this).
▪ If the baby is compromised at birth encourage the parents to talk to their baby whilst the placental circulation re-establishes the normal blood volume and oxygen for the baby (do not cut the cord to remove baby for resus).
The baby in the photo above was born at home into water. His cord was tightly around his neck twice. The midwife is in the process of unwinding the cord whilst bringing him to the surface and into his mother’s arms. He took around a minute to start breathing whilst his placental circulation re-established his blood volume and oxygen. His father gently blew on his face and he took his first gasp.
You can see a lovely example of a baby being born with a loose nuchal cord (and in the caul on Pamela Hines’ website.
Gloria Lemay has posted some photos of a baby being born with a multiple nuchal cord here.
The somersault manoeuvre
I have only had to use this twice in hundreds of births.
For many more thought provoking and informative blog posts on mothers, babies, birth and midwifery, head over the Midwife Thinking blog or keep up to date with the latest posts by following Midwife Thinking on Facebook.
Do you have your own birthing story involving difficulty with a nuchal cord?